Items filtered by date: June 2022
Risks of Stress Fractures in the Foot

Anyone who is active physically on a regular basis is a prime candidate for stress fractures. Among the main causes of these hairline cracks in a bone are changing your workout program, improper footwear, and improper technique. Going from running on turf to running on a road or other hard surface also may put you at risk. High-impact sports, such as soccer, running, basketball and dance, increase the likelihood of sustaining stress fractures. Non-athletes can also develop stress fractures, usually by increasing activity after refraining for a long time. Having osteoporosis and vitamin D deficiency, especially common among postmenopausal women, is another risk factor. If you have sustained stress fractures in the past, you are more likely to experience them again. If you suspect you may have developed stress fractures in your feet, it is a good idea to consult a podiatrist who can conduct a thorough examination and offer appropriate treatment options to reduce your pain.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Dr. Mark Gagnon from Advanced Podiatry. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Risks of Stress Fractures in the Foot

Anyone who is active physically on a regular basis is a prime candidate for stress fractures. Among the main causes of these hairline cracks in a bone are changing your workout program, improper footwear, and improper technique. Going from running on turf to running on a road or other hard surface also may put you at risk. High-impact sports, such as soccer, running, basketball and dance, increase the likelihood of sustaining stress fractures. Non-athletes can also develop stress fractures, usually by increasing activity after refraining for a long time. Having osteoporosis and vitamin D deficiency, especially common among postmenopausal women, is another risk factor. If you have sustained stress fractures in the past, you are more likely to experience them again. If you suspect you may have developed stress fractures in your feet, it is a good idea to consult a podiatrist who can conduct a thorough examination and offer appropriate treatment options to reduce your pain.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Dr. Mark Gagnon from Advanced Podiatry. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Rheumatoid Arthritis Affects the Feet
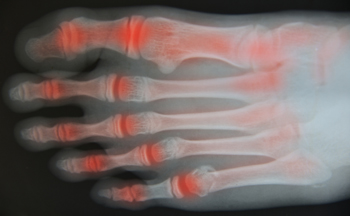
Experts say that 90 percent of people with rheumatoid arthritis (RA) will experience problems with their feet and ankles. Inflammation from this disease causes pain, swelling, redness and a limited range of movement in the joints. In addition, the cartilage, ligaments, and tendons are broken down by the immune system. This, in turn, may cause difficulty in standing and walking for long periods of time. Rheumatoid arthritis can affect the ankle by making it more difficult to go up and down steps. In the hindfoot area, RA impedes the ability to walk on uneven surfaces, such as gravel. Pain generally starts on the outside of the foot, and eventually moves to the arch and the inside of the foot. It may even lead to flat feet as bones shift and become damaged. In the midfoot, the ligaments that support the feet become weaker and cause a collapse of the arch. Deformities in the toes, such as bunions and hammertoe, caused by rheumatoid arthritis may make it difficult not only to walk, but to wear shoes. If you have rheumatoid arthritis, it is a good idea to develop an ongoing relationship with a podiatrist to monitor these and other changes to your feet and ankles.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Mark Gagnon of Advanced Podiatry. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Rheumatoid Arthritis Affects the Feet
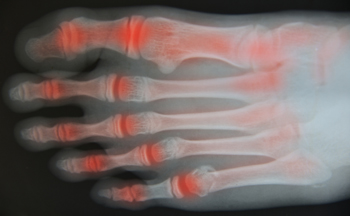
Experts say that 90 percent of people with rheumatoid arthritis (RA) will experience problems with their feet and ankles. Inflammation from this disease causes pain, swelling, redness and a limited range of movement in the joints. In addition, the cartilage, ligaments, and tendons are broken down by the immune system. This, in turn, may cause difficulty in standing and walking for long periods of time. Rheumatoid arthritis can affect the ankle by making it more difficult to go up and down steps. In the hindfoot area, RA impedes the ability to walk on uneven surfaces, such as gravel. Pain generally starts on the outside of the foot, and eventually moves to the arch and the inside of the foot. It may even lead to flat feet as bones shift and become damaged. In the midfoot, the ligaments that support the feet become weaker and cause a collapse of the arch. Deformities in the toes, such as bunions and hammertoe, caused by rheumatoid arthritis may make it difficult not only to walk, but to wear shoes. If you have rheumatoid arthritis, it is a good idea to develop an ongoing relationship with a podiatrist to monitor these and other changes to your feet and ankles.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Mark Gagnon of Advanced Podiatry. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The Achilles Tendon Controls Pointing and Flexing the Foot

The large tendon located in the back of the calf is known as the Achilles tendon. It plays an important role in pointing and flexing the foot which is vital to completing daily activities. An Achilles tendon injury can occur for several reasons. These can include sustaining a running or jumping injury, changing an exercise routine, or wearing shoes that do not fit correctly. There may be existing medical conditions that lead to this painful foot condition, including obesity, having flat feet, or if your foot rolls inward while walking or running. The symptoms that are often associated with this type of injury can consist of intense pain at the time of the injury and stiffness, and the affected area is often swollen. Some patients even hear a popping noise as the injury occurs and this generally requires immediate medical attention. There are different methods to treat this condition and it is strongly suggested that you are under the care of a podiatrist who can determine which treatment is best for you.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Mark Gagnon of Advanced Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Achilles Tendon Controls Pointing and Flexing the Foot

The large tendon located in the back of the calf is known as the Achilles tendon. It plays an important role in pointing and flexing the foot which is vital to completing daily activities. An Achilles tendon injury can occur for several reasons. These can include sustaining a running or jumping injury, changing an exercise routine, or wearing shoes that do not fit correctly. There may be existing medical conditions that lead to this painful foot condition, including obesity, having flat feet, or if your foot rolls inward while walking or running. The symptoms that are often associated with this type of injury can consist of intense pain at the time of the injury and stiffness, and the affected area is often swollen. Some patients even hear a popping noise as the injury occurs and this generally requires immediate medical attention. There are different methods to treat this condition and it is strongly suggested that you are under the care of a podiatrist who can determine which treatment is best for you.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Mark Gagnon of Advanced Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What is Diabetic Neuropathy?

Many people who have had diabetes for a long time may also have a condition known as diabetic neuropathy. The most common form is peripheral neuropathy, which in diabetics usually affects the feet. Symptoms include numbness, reduced ability to feel pain or temperature changes, and tingling or burning sensations. Sharp pains or cramps may also occur. These can further evolve into foot ulcers (wounds that do not heal properly) and infections from cracks or sores in the skin. If ignored or left untreated, gangrene may develop which could lead to surgery or amputation. The main causes of peripheral neuropathy are high levels of sugar and triglycerides in the blood which can damage the nerves and blood vessels in the feet. Since the symptoms of peripheral neuropathy develop over time, it is easy to overlook this condition. Daily foot care is imperative to maintain healthy feet. Another important way to prevent or handle diabetic neuropathy is to schedule regular visits to a podiatrist who can monitor the condition of your feet and treat them accordingly.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Dr. Mark Gagnon from Advanced Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Diabetic Neuropathy?

Many people who have had diabetes for a long time may also have a condition known as diabetic neuropathy. The most common form is peripheral neuropathy, which in diabetics usually affects the feet. Symptoms include numbness, reduced ability to feel pain or temperature changes, and tingling or burning sensations. Sharp pains or cramps may also occur. These can further evolve into foot ulcers (wounds that do not heal properly) and infections from cracks or sores in the skin. If ignored or left untreated, gangrene may develop which could lead to surgery or amputation. The main causes of peripheral neuropathy are high levels of sugar and triglycerides in the blood which can damage the nerves and blood vessels in the feet. Since the symptoms of peripheral neuropathy develop over time, it is easy to overlook this condition. Daily foot care is imperative to maintain healthy feet. Another important way to prevent or handle diabetic neuropathy is to schedule regular visits to a podiatrist who can monitor the condition of your feet and treat them accordingly.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Dr. Mark Gagnon from Advanced Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.